To understand how strabismus surgery works, consider that each of your eyes has six outside (extraocular) muscles controlling eye movements.
If a muscle is too strong when you have strabismus, it may cause the eye to turn in, turn out or rotate too high or low.
On the other hand, an eye muscle weakness in certain cases may also cause misalignment. This condition may occur if you have a
dysfunction affecting how eye muscles control movement.
Fortunately, your ophthalmologist has various surgical options to help correct these types of problems.
Strabismus Surgery Involving Recession And Resection Procedures
In a recession procedure, your eye surgeon detaches the affected outside muscle (extraocular muscle) from the eye and reattaches it (resection) farther back on the eye to weaken the relative strength of the muscle if it is too strong.
In contrast, if the muscle is too weak, your surgeon may use a recession procedure to reduce strength of the opposing muscle (antagonist) to achieve more balanced function of the eye muscles.
In certain cases, a resection procedure may be used to strengthen an eye muscle to correct misalignment associated with strabismus. If you have inwardly turned eyes (
), the surgeon may strengthen the lateral rectus muscles — located on the side of each eye, toward the ear — by reattaching the muscle in a different location (resection). In this way, the lateral rectus muscles are relatively strengthened and they can turn the eyes farther outward. This results in better eye alignment.
Adjustable Suture Strabismus Surgery
With adjustable suture eye muscle surgery, your surgeon adjusts sutures holding eye muscles in place after a resection procedure, to attempt to improve your final outcome.
Generally this surgery is possible only in adults, with perhaps only a small percentage able to benefit. This surgery is probably best for someone in whom strabismus developed in adulthood after previously normal eye alignment.
In this case, the person is a good candidate because of fusion potential — the ability of both eyes to “lock on” to a target simultaneously, resulting in stereovision and a high degree of depth perception.
In most cases, adjustable suture surgery is performed in the operating room, with general or local anesthesia. Afterward the eye is patched. About four to 24 hours later, the patch is removed in the office, when anesthesia and sedation have faded. Ocular alignment is then evaluated.
Based on how your eyes are aligned, your surgeon may decide to use the suture that is in place to tighten or loosen the treated muscle. This adjustment may cause slight discomfort, primarily with muscle tightening.
Once the desired alignment is achieved, the surgeon ties the adjustable suture permanently in place, and the procedure is complete.


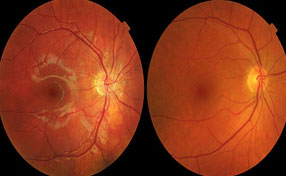
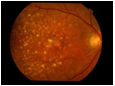 Dry: Most patients with macular degeneration suffer from the dry form of the degeneration producing a gradual weakening of the retina. This can be seen as yellow deposits in the retina called Drusen or as areas of increased or decreased pigmentation of the retina. It is important to have the eye examined as for some types of dry degeneration (for example the eye on the right) special vitamin and antioxidant tablets have been found to reduce the risk of progression to visual loss.
Dry: Most patients with macular degeneration suffer from the dry form of the degeneration producing a gradual weakening of the retina. This can be seen as yellow deposits in the retina called Drusen or as areas of increased or decreased pigmentation of the retina. It is important to have the eye examined as for some types of dry degeneration (for example the eye on the right) special vitamin and antioxidant tablets have been found to reduce the risk of progression to visual loss.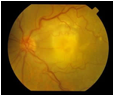 Wet: A few patients will produce a more severe form where a blood vessel membrane appears in the eye as shown on the left. This causes damage to the retina with severe loss of vision often in both eyes. In the early stages the vision distorts followed later by loss of central vision.
Wet: A few patients will produce a more severe form where a blood vessel membrane appears in the eye as shown on the left. This causes damage to the retina with severe loss of vision often in both eyes. In the early stages the vision distorts followed later by loss of central vision.